Member Stories
People with Erythromelalgia, and those who think they have EM, can gain from reading other people’s experiences with the condition. The road to diagnosis is often long, and coping with EM can be difficult. People with EM all have a story.
Sierra Domb

Los Angeles, CA
My name is Sierra Domb, and I’ve lived with Erythromelalgia (EM) and co-occurring autoimmune issues since childhood. My symptoms include burning pain, swelling, redness, and heightened blood flow surging through my hands and feet. Although I enjoyed being outdoors and staying active, these activities were often difficult for me. Heat and movement increased my body temperature and blood flow, which triggered pain and discomfort.
I didn’t have a name for what I was experiencing, and no one around me had heard of EM. When I tried to explain my symptoms, I was often met with bewilderment, and the visible effects EM had on my appearance were frequently met with shock and a lack of compassion.
Unfortunately, many children and adolescents with chronic conditions are not taken seriously. Their symptoms are often dismissed, and the difficulty of managing school, responsibilities, and social life while dealing with ongoing health issues is frequently overlooked. Instead of receiving support, pediatric patients are often misunderstood or told they are “too young” to have serious health problems, leaving them feeling unseen and isolated for not matching the expected image of a healthy, carefree young person. This expectation doesn’t reflect the reality that anyone, regardless of age, can face health challenges.
It wasn’t until young adulthood, while seeking medical attention for the sudden onset of Visual Snow Syndrome (VSS), that I was formally diagnosed with EM. During testing, doctors noticed the redness in my hands and feet, leading to further evaluation and tests that confirmed EM.
With a background as a neuroscience research collaborator and health communicator, I’ve focused on understanding how the brain and nervous system influence EM. By supporting key brain systems, such as the hypothalamus, pituitary gland, and autonomic nervous system, I’m better able to manage heat sensitivity, pain fluctuations, hormonal changes, and autonomic imbalances that trigger flare-ups. Evidence-based practices that reduce stress, promote homeostasis, and harness neuroplasticity, like mindfulness, have also helped me decrease pain sensitivity and build resilience.
I also manage my symptoms by staying cool whenever possible, consuming or gently applying chilled water as needed, portable fans, umbrellas for shade, and keeping my sleeping environment cool to prevent worse flare-ups and insomnia. Some medications have no effect, while others worsen symptoms or cause side effects, though experiences vary by individual. Although flare-ups are sometimes unavoidable and life doesn’t always allow perfect management, I’ve learned what to expect and what helps me cope.
I’m sharing my story to raise awareness. If you’re navigating EM, especially as a young person, and feeling discouraged, know that while you may face challenges others don’t or need extra steps to stay comfortable, you can still find moments of happiness and lead a fulfilling life. I experience medical challenges, but the strength EM has required me to build has also made me more compassionate, knowledgeable, and resilient in managing my condition and navigating life. If anyone, including a doctor, lacks patience or compassion, they may not be the right fit for you. It can take time to find those who truly accept you as you are, but they exist. Do not try to be someone you’re not or minimize your experience just to please others. In a world obsessed with productivity and the illusion of perfection, self-acceptance, authenticity, and self-care are actually some of the most productive things you can do. Life is hard enough, especially when facing a chronic condition. Whether you are struggling or not, whether you have EM or know someone who does, be kind to yourself and to others.
Erika Conrad
Tacoma, WA
I am 19 years old and though I’ve had EM for about 10 years, I was only diagnosed a couple of years ago. I haven’t found any medication that helps the pain in my feet. The doctor now has me on Neurontin and Tramadol and I hope they help. Now even my face gets extremely red and hot when I am very stressed. I rarely leave the house due to the pain, which seems almost constant. I wish I had someone in my life who understands, but EM is almost impossible to describe. I’ve applied for disability, which I really need since I cannot work. I recently went for a walk with my three-year-old daughter to get some fresh air. She had been begging to go out for a week. After about 15 minutes, she suddenly said her feet hurt. We sat down at a bus stop and I just started crying when I thought about her little feet hurting the way mine do. On the way home, I stopped at our mailbox and found TEA’s FootSteps. When I read others’ experiences with EM, it was comforting to know that I’m not alone and there actually are people out there who understand and want to help. Erika lives in Tacoma, WA. You can email me at EJC9121@Yahoo.com
Irene Kellough
As a new TEA member and am so happy to know that I am not alone with EM. I am an 89 year old widow living alone, but fortunate to have family nearby. My EM started about six years ago.
I noticed a TEA member once asked if anyone experienced EM stopping during an illness or injury. When I fractured my right ankle two years ago, my feet stopped hurting for about 10 days, then returned worse than before. Now I flare constantly. My right foot and ankle where the skin was damaged is very sensitive, dry, swells more and stiffens when I stand. I also have heel cracks and toenail problems, heavy freckling on the front of my legs, ankle to knee, darker on my ankles, but no discomfort there. I wonder if others experience this.
I’m using creams, a camphor, as recommended by some members, fans, air conditioner and cool wraps at night, but, sleeping is still difficult. I keep my shoes and socks in the refrigerator.
I enjoy reading and doing crossword puzzles. I have been volunteering at a nursing home for over 15 years. I like to speak on the phone with family and friends. I also keep busy with housework, grocery shopping, and doing exercises in my home. And, of course, I spend a lot of time trying to keep my feet cool…a full time job!
But, I am happier and grateful to be part of the TEA group and thank everyone for their support.
I would welcome hearing from others at anytime (416-694-8313).
Jean Warwick
Oxford, England
My problem began four years ago when I was 73, shortly after a knee replacement operation. I have all the usual EM symptoms—burning feet and lower legs with redness, swelling and flare-ups, but also only the back of one hand. All are worse at night. I can’t walk or stand for long as the pain increases to the “razor blades” sensation in the soles of my feet. My bedroom is unheated even in winter. I can only take paracetomol or co-codamol (for sleep) as my stomach does not tolerate aspirin- based medication.We tried the tricyclic antidepressants, but I was like a zombie. I now take 20 mg citalopram, which helps a little. The skin on my legs and feet is very dry and flaky and I have rashes which defy all creams. I am always tired and cannot do many of the things I used to do. I go barefoot inside and wear sandals outside, even in the snow here in Oxford, England. My husband of 59 years is very supportive and, being a Quaker, I have many Friends who commiserate with me and are very kind. Most people’s eyes glaze over when I try to answer their questions, including local doctors. Nobody really understands the causes or knows what to do. I just soldier on and very bravely (I think). I have agreed to go on a train trip across to Greece and the Island, as I refuse to let my EM win. I imagine that I shall see more of the hotel lounges than the museums and antiquities!! I have been assured that there is air conditioning!
Audrey C. Moser
Portland, OR
I’ve never felt better in my life, more powerful or more in control and I want to share about learning a practice of “Riding the Waves.” As I faced another summer, confined alone to my upstairs condo, sitting in front of the air conditioner until the outside temperature would get below 70 degrees and I could go outside, my usual, uninvited, annual depression began to take hold.
Then, in early May 2011, while attending my weekly “Easing into Yoga” class, my teacher Kimberly Carson spoke about a new class she is teaching – “Yoga of Awareness for Chronic Pain.” She described the eight-week sessions – two-hour classes, based on gentle stretching, meditation, breathing practices, combined with the exploration of yogic wisdom and study of the relationship among yoga practice, experiences, and management of pain. She described all sensing as happening in waves and learning to “Ride the Waves” is imperative. Being definitely aware that I lived with chronic pain, I signed up.
The first class was May 6, 2011, and lo and behold, within two weeks, I needed no pain meds for my chronic pain. After learning a three-part breathing technique that enabled me to breathe through the onset of the first twinge of forthcoming horror, I was able to conscientiously and calmly “ride the waves” of sensing and tune into just being, and the twinge diminished and disappeared. The exploration of a different way of thinking about my pain and training my mind to respond differently to the stress, fear, and hopelessness that had accompanied my past five-year struggle living with EM is exciting and remarkable. It isn’t easy or simple, but takes daily yoga practice, meditation, and concentration. I’m still in a learning process, still tuning into “riding the waves.” The practice has produced marvelous results with my chronic pain and when used in response to acute pain, a softening and deepening peace ensues. As I write, summer is here and not one day has found me confined. I continue to seek shade, use some common sense, and take my daily medicinal routine of gabapetin, Zoloft, and Zyrtec.
This incredible class of empowerment was developed by Kimberly Carson, MPH, RTY health educator, specializing in mind-body integration. She works as a yoga therapist, mindfulness teacher, and teacher trainer at OHSU and Duke University Integrative Medicine.
P.S. It’s January 2012 and I’m still “Riding the Waves,” still amazed and delighted with the calming results and still pain-med free (other than an occasional Advil). Audrey lives in Portland, OR, USA, may be contacted at acmoser2@juno.com
NOTE: TEA does not endorse the classes or services of Kimberly Carson, MPT, RTY.
Susan Alexander
I first discovered my unusual foot condition in 1994. I remember it well because it was another significant benchmark in my life. I had just moved to another town with my fiancé where we both had started new jobs. I remember coming home after work wondering why my feet were aching, red-hot, and at times unable to support me. I thought it was from standing on them while working a retail job. Knowing nothing about this condition, but seeking relief of any kind, I would soak my feet in hot water and prop them up on a pillow at night. No amount of pampering gave much relief. After eight months of stress and incompatibility with my fiancé, I ended my relationship and took my belongings and my fire-infested feet back home.
I saw a podiatrist who had never heard of my symptoms. He proceeded to give me cortisone injections in my arches. The problem went away for a few months or so. After another year of suffering I went to another podiatrist and he said that he had seen these symptoms one other time in a very young girl. He told me that an antihistamine worked for her and gave me a prescription for Claritin. Surprisingly it did work; however, I didn’t think it was healthy to keep taking the medication year round, so I only took it in the summer months. Over the years my body has built up a tolerance to it.
I’ve continued this process through today. I have learned that my EM is exacerbated by the temperature outside, my body overheating, all-over body lotion, and stress. It has really been a challenge to exercise or enjoy summertime outdoor activities with this condition. I joined TEA this year and I really want to start a fundraiser here in Columbus, Ohio, for those suffering with EM. I have recently purchased some clothing with a pattern of feet on them. I get asked all the time, “What’s up with the feet?” This opens the door for me to tell them about my EM. It is part of my life’s work to educate people about this condition.
Susan Johnson
My EM started right after my daughter’s wedding in Texas in 2006. Before returning to California my feet started burning. I thought I had caught an infection and searched drug stores for anything I could find to cool them. This is when it all started. Little did I know from that day forward I would never be the same person.
Several weeks passed before I made an appointment to see the doctor. My feet would turn blue without reason, then reddish purple and burn so much it would make me sick. At first I was diagnosed with neuropathy and later a neurologist diagnosed “Hot Feet” and said, “I don’t treat this.” I left the office in tears. I was then referred to another neurologist who has treated me for three years. I give him every bit of information on EM that I can find. It seems since there is so little known about this rare condition that I still feel left out, medically. My world has come to an inactive halt. I have to plan my days, interests and my life. I find that ice packs are my savior.* I have started playing pool, which surprises me. But, I find it quite enjoyable for one that has to have a cool room temperature. This can be played all year round. I also have a wonderful spouse who helps me and tries to understand this strange event that has happened to our lives. I know that he will never understand the total pain of EM.
I am now taking Methadone 5mg, Lyrica 250mg, and Cymbalta, all twice a day. I have tried many other drugs, but they didn’t help. These three drugs still are not covering my pain either. I will have to talk to my doctor again to see what we can do. Weight gain seems to be a big problem. The medication along with EM slows you down considerably. Walking in a swimming pool is grand. Trying to walk the dog is very painful.
*EDITOR’S NOTE: Using ice packs is not recommended by doctors.

Doreen Senior
San Jose, CA
I was diagnosed with EM four years ago. Several months after undergoing arthroscopic surgery on my knee, I noticed that my toes were red, warm and tingly. Neither the orthopedic doctor nor my regular doctor had any idea what was going on, so I was referred to a neurologist. He determined that I wasn’t suffering from any neurological problems, so the mystery remained. Eventually another doctor finally diagnosed EM, after some lengthy consultations. I laughed to myself at the time thinking that I managed to get something that I had never heard of, nor could pronounce or spell.
I worked at a large school district for almost 30 years, starting as a school secretary. I later became part of the purchasing team, finally becoming the District Purchasing Agent.
I am retired and live in an active senior community in San Jose, Calif., called “The Villages.” Although EM has impacted my life considerably, I mostly keep it to myself. People will ask me “Are your feet better?” and when I say, “No,” I often wonder if they believe me. I also get asked “Why are you wearing sandals playing golf?” or, “Aren’t your feet cold in those sandals?”
I believe that staying busy helps me to temporarily forget my EM problems, so I’m very involved with activities in my community—serving as an Emergency Preparedness Chief, doing the handbook for my golf group, creating tickets and programs on my computer for several other groups at The Villages, and singing with the Village Voices.
I am single, have three grown children and four grandchildren. I have been writing my memoir and have taken classes on memoir writing. Regarding EM, my vision is to help make more information and research available to everyone.
Heather Demars
My battle with Erythromelalgia began in September of 2012. I was walking barefoot in my backyard and felt a sharp pain in the ball of my right foot. I thought I had been stung by a bee, but after limping inside and inspecting my foot, there was no sign of a sting or any other injury. I hobbled around for the rest of the night, figuring it would be better in the morning.
It wasn’t.
I woke up in the middle of the night with the toes of my right foot feeling like they had been scraped raw. I stumbled into the bathroom, wondering what on earth I had done to my foot while sleeping, but again, my foot looked completely normal. Over the next several days, pain spread to all of my toes and then throughout the rest of my right foot, then started in my left foot. My feet still looked normal at this time, but felt like they were burning, being stung by bees, and being electrocuted all at the same time. The bones of my feet ached and felt broken, and the joints felt stiff. It became almost impossible to walk and the only thing that brought relief from the excruciating pain was keeping ice packs on my feet almost around the clock.
Though I saw numerous specialists and doctors, nobody could tell me what was happening. X-rays, nerve conduction studies, biopsies, blood tests, MRIs, and countless other tests all came back normal. But my pain was off the charts, constant, and now my feet were turning red and swelling. No pain medications helped. At one point I was on ten medications at once, and all it managed to do was make me groggy. I was on long- and short-acting morphine, plus hydromorphone and lorazepam among many others. Later a pain specialist told me that with that combo it was a miracle that I hadn’t died. At the height of my pain, I was hospitalized and given a full epidural. For the first time in months, the pain went away completely. I burst into tears of relief! But two hours later, the pain of EM broke THROUGH THE EPIDURAL. At this point I lost all hope that anything could help.
After 8 days in the hospital, the combination of the epidural, IV lidocaine, and IV hydromorphone finally relieved the pain to the point that I could go home on oral narcotics and Carbamazepine. The pain was still horrible, but was down to about a constant 7. Over the next couple of months the pain gradually improved to the point that while I still flared daily, the pain rarely got over a 6 or 7.
We finally linked the onset of my EM to use of the drug Ciprofloxacin, and while I wish every day I had never taken that drug, I also know that I have learned and grown in ways from this trial that I wouldn’t have been able to in any other way. I currently manage my pain using only 30 mg. of Cymbalta daily, and lifestyle modifications like not wearing socks or shoes (only flip flops), elevating my feet and cooling with a fan, sleeping with a fan blowing on my feet at night, trying to avoid temperatures below 45 degrees (F) and above 70 degrees (F), and avoiding too much time on my feet. Stress, lack of sleep, and sugar can also trigger flares. As a wife and mother of three (ages 4, 11, and 16), it’s not always easy to avoid flares and pain. But for the most part I try to respect my body’s limits and focus on what I still am able to do.
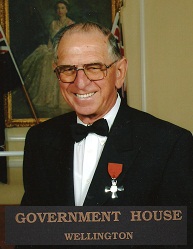
Bill Bracks
Te Puke, New Zealand
I live in Te Puke, New Zealand. I’m 80 and finally retired from my job as a company chairman. My first symptoms appeared with hot, swollen, burning feet 25 years ago. I photographed them for my GP who could not diagnose or research the complaint. So, I was off to numerous consultations with specialists. The burning feet were preferable to their prescriptions. I finally decided what you cannot cure you must endure! In the early days I would get out of bed and stand on the tile floor to get some relief and hopefully sleep. I also found that bare feet on the lawn brought relief and do believe there is a relationship to the level of the zeta potential (the negative electrical charge on which our body functions), e.g., when you wear shoes or are lying in bed your body is not earthed and the natural negative 15 to negative 100 millivolt charge becomes supercharged and out of balance. Colleagues at board meetings often passed snide remarks about the Chairman being unable to afford shoes when I was sitting barefoot in meetings. If only they knew!! You cannot feel others’ pain and in the case of EM it is even more so. My remedy today is off with the shoes and socks as soon as is practicable. If that means having worn them for three or four hours, then it’s a bowl of cold water to cool them down before retiring or a stroll on the lawn if the weather allows. In bed, cold wet towels keep my uncovered feet cool enough. Not an ideal situation but it makes life a little more bearable. I do have a carbon fibre underlay which is coupled to a copper earth rod outside the bedroom window. I believe this also helps. When undergoing a recent heart valve operation it was a nightly fight with the nursing staff to let me keep my feet sticking out of bed. My sympathy goes out to all those who suffer from this rare disease. It is fantastic to have a dedicated band of people in TEA who care enough to form this worldwide association. The idea of forming support groups in countries outside the U.S. may just be the best means of accessing the resources to fund more research into this nasty condition. Blessings from Kiwiland.
Jane Beattie
Oceanside, CA
Since the early ‘80s, I‘ve had symptoms of peripheral neuropathy, specifically tingling spreading from my hands and feet. EM showed up in 2008 (at age 60) while walking around Rome for 10 days. (At least it was a fabulous trip!)
I always have swelling in my hands and feet, which gets worse when they are hot. There are a couple deep cracks on each of my feet. I have to ration the amount of time I spend using my hands and feet. I try to minimize contact with water. For several months I got very little sleep. When I changed my meds to 100 mg amitriptyline and 5 mg zolpidem tartrate (Ambien), I was able to stay in bed with only occasional applications of freezer-chilled “Hot Pockets.” I mention “Hot Pockets” because I have found them to be the gentlest coolant (aside from fans). They are cloth beanbags designed to put around your shoulders. I found mine at a drug store. You need several because they don’t keep their cool for long (pun intended). When my feet get super-heated, though, the only thing that cools them down is a plastic cold pack from the freezer—with an old kitchen towel between the cold pack and my skin. (EDITOR’S NOTE: The use of ice packs is not recommended.)
Skin care is also a problem for me since getting EM. I’ve found a routine that seems to work. After a quick lukewarm shower, I use a hypoallergenic lotion on my body (Aveeno with colloidal oatmeal). Eucerin cream works well on my feet, after which I put on clean cotton socks. I keep the socks on until my feet start to “complain” (the tingling that precedes the heating up). For body soap and shampoo, I use Johnson’s natural head-to-toe foaming baby wash. I’ve found the baby section is a good place to shop for gentle products.
(Jane lives in Oceanside, Calif. USA)
Starla Jackson
I’ll never forget awakening with EM last April. The symptoms have not ceased for a second. My hands and feet feel as though I am being stung by a hellacious jellyfish while simultaneously being placed in an open flame. I’m sure this is common. I tried months of Lyrica, Neurontin, and Chinese herbal capsules, none of which helped at all, as well as topical remedies—some prescribed and some of my own concoctions. I don’t know how I ever found time to work. It seems that being disabled is at least a 60 hour per week job.
I use Lidoderm (five percent lidocaine) patches on other areas, and one day I slapped those on my feet just for the heck of it. They helped some. When I told my “brilliant” neurologist this, a light bulb went on. Oral lidocaine (Mexitil) had been relatively recently developed for heart patients. He put me on 150 mg twice daily. I felt some relief within 48 hours. After a week, I would say the burning was relieved by 40 percent. At least I was no longer suicidal nor was I desperate to amputate my limbs.
After 30 days of Mexitil at this dosage, he increased it to three times a day. However, I have not noticed any further relief.
Mexitil does have side effects. The primary one is nausea, which has not affected me one iota. What has affected me is extreme exhaustion as well as a bit of dizziness, but it’s definitely a good trade-off.
I am a widow with no children. However, I “claim” hundreds of children—my piano students. I have a Master of Music and served as a college piano faculty member, as well as operating a private piano studio, “Starnote Music.” My most recent position was with the Houston, TX, Grand Opera. I’m now retired, due to my multiple neuro-progressive disorders. I am an avid baseball fan and peace activist. I’m also a volunteer pianist—even with slightly burning hands.
(Starla would like to correspond with other members. See Member Directory for her email address or phone number.)
Martha Davis
I wanted to share my experience because, after reading so many accounts of others, I feel so blessed. I was in my 60s before really paying attention to the weird symptoms I was having—intense burning of my face, one ear, and /or my hands. I passed it off as hormones, but at age 70, I began to have terrible itching in my feet, primarily at night. I was not sleeping and saw my primary physician for help. He tried several medications but finally sent me to various specialists, but got no help. On the advice of a cousin, I went to Arthritis Centers of Dallas and saw Dr. Christopher Tehlirian. After blood work and urinalysis, and bringing in other doctors to look at my red, swollen feet, he diagnosed EM. Because of some protein in my urine, he sent me to the Oncology Department at Baylor Hospital for more testing. Baylor ruled out lymphoma, so EM was the primary diagnosis. Next I had a biopsy of my foot, which showed clusters of white cells. Previously, Dr. Tehlirian had told me to take one aspirin at night and also put me on gabapentin. I had some relief, but not much. He then added magnesium citrate. This really helped. I was still having episodes so Dapsone was added to my regimen. I have been sleeping all night since taking two a day. The fact that I went to Dallas was answered prayer—nothing else! Dr Tehlirian (a Johns Hopkins grad) told me he liked a “challenge.” This strange ailment is not in his field, but I will be forever grateful for his persistence and determination. I hope this information helps someone.

Jules Hunter
Noosa, Queensland, Australia
I am 42 years old and was diagnosed with EM in September by a rheumatologist here in Noosa, Queensland, Australia, which is one of the warmest states in “OZ”. However, I would not live anywhere else but this special part of the world. I also have multiple sclerosis.
The burning started in my feet about four years ago. Exercise, walking, heat, and hot showers bring on the burning, throbbing, pain. This also occurs at night when resting, even without a sheet or blanket. I use A/C, a fan, and elevate my feet for relief and only wear open-topped sandals. I also have flares in my knees and on patches of my face and ear.
In high school, I played many sports and was on a music scholarship. I now know why I had burning pain, numbness, paralysis, vertigo, immense fatigue and frustration when unable to achieve my goals. I pushed myself more, thinking it would help. I’m no longer able to work, but I earned my diploma in Financial Planning two years ago.
I am able to cope with the MS as I know I can keep symptoms under control with diet, rest, exercise and limiting stress. I cannot control EM as easily. The pain and burning interrupts my love of walking and the lack of sleep is cruel. I’m sure many of you can relate. I was told I was given MS and EM as “gifts” because I can cope, with my positive attitude and love of life, which is so true.
When I meet people, the common response is “Oh, but you look so good you would never know.” My Mum always taught me “if you look good (which I always try to do), you feel good”. I love my life and wake each day in anticipation of what it will bring. Simple things like having coffee with my beautiful Mum and walks along the beach make me so happy. The support I have from my parents and close friends encourages me to achieve my goals.
I am so impressed with TEA, the staff, doctors and incredible range of articles available. My doctors and pharmacist refer to these constantly.
TEA was saddened to learn that Jules took her own life in 2016 after both her MS and EM had deteriorated. She is survived by her parents, Simon and Sue Wischer. Read article.

Mary Ann Coplin
I am 62 yrs. old, married, and have an adorable 6 yr. old baby girl, named Brie Marie, my mini schnauzer. My battle with EM began in my late 30’s, when I started to experience intermittent symptoms of burning pain, and swelling in my hands. At the time, little did I know just how much my normal life was about to change.
My symptoms gradually became more chronic with a constant burning pain in my feet, especially on my heels. My hands started to exhibit Raynaud-like symptoms. I have learned that I have autonomic dysfunction, which causes me to be extremely reactive to pain in general, and a very low tolerance to cool and warm temperatures.
I finally received my EM diagnosis and small fiber/peripheral neuropathy by Dr. Mark Davis at the Mayo Clinic. I attended a 3-week Chronic Pain Program there, which was somewhat beneficial, but also overwhelming. In 2013, I was genetically tested, indicating that I carry the primary gene and other unknown variant genes. I also have facial EM.
I have tried every treatment offered to me, from oral and compounding medications, to infusions, nerve blocks, and even a spinal cord stimulator implant. Unfortunately, they have all been unsuccessful because I either could not tolerate the side effects, or they were ineffective.
I have found that the best therapies for me in easing my stress and calming my mind and body are Viniyoga, deep breathing, meditation, an online support group, and striving to accomplish something positive every day. I find that distractions of any kind are effective because they engage me to become involved and to concentrate on something other than myself. I also enjoy collecting inspirational articles and sharing them with others, as well as random acts of kindness. My husband is my rock, and my ultimate goal is to be able to hold hands with him again.
I would encourage every member to consider becoming a volunteer for TEA. The need is great, and I, personally, have found it to be a very rewarding experience. We are a unique group of people who have the ability to reach out and touch each other by lending a helping hand in any way that we can. What better way to add value and purpose to your life than to make a positive difference by contributing to the cause of TEA and your fellow members.

Danni Wortmann
Hartington, NE
Prior to developing erythromelalgia I enjoyed a busy life raising our children and helping my husband on our farm. We did a little traveling and I enjoyed walking several miles a day. I used to do calligraphy as well. I enjoy swimming and still am able to do this a few times each week in an indoor pool as I am unable to outside in the heat for too long.
Having the terrible burning pain, not only in my hands and feet but full body, has changed who I am and what I do. Making plans too far into the future is hard as I never know how I will feel.
I used to love spending time outside in the summer. During the winter I loved to ice skate but am no longer able to do this.
My husband Ron and I have been married 34 years and we have a farm in Northeast Nebraska. We raise cattle, hogs, corn, soybeans and alfalfa. I’m grateful my husband is a very hard working, loving and considerate person. He has helped me tremendously in dealing with EM. Our son Nathan is a firefighter/paramedic in Norfolk, Nebraska. Our daughter Katie is married and lives in Omaha, Nebraska where she works as director of marketing and public relations for Opera Omaha. We are so blessed that our children love their jobs and are successful in what they do.
I have a Master’s degree in Nutrition from University of Nebraska at Lincoln and have worked part time as a dietitian. With this EM, I now focus on things I can do, such as; visiting and calling friends and reaching out to others in need.
(Danni is a TEA volunteer and in charge of mailing the bookmarks.)
Anonymous Member
San Francisco, CA
My EM started when I was 41, as a direct result of bilateral tarsal tunnel syndrome (TTS). I also believe that my use of ice packs for my TTS contributed to the onset of EM. It came on gradually, and after having been misdiagnosed by one doctor with CRPS/RSD, I tried hyperbaric oxygen therapy. Instead of helping, the increased blood flow from the treatment caused my EM to suddenly become very severe. I went from using cool washcloths and a fan to soaking my feet in cold water almost 24/7.
I desperately tried a number of medications and supplements. None helped and some caused my flaring to worsen significantly. I had been bedridden for almost a year when I finally found some relief. In 2013, I had my first Qutenza (8% capsaicin patch) treatment with Dr. Wendye Robbins at Stanford. This gave me about a 50% reduction in my EM symptoms! Finally, I could get rid of the water buckets and ice packs and only needed a fan for cooling.
Over the next couple years, I had two more Qutenza treatments, but neither gave me further relief. In 2015, I tried Will Prowse’s protocol, which involves OTC capsaicin cream applications, followed by a period of progressive heat exposure. After a few treatments, my EM did improve to the point where I could tolerate hot showers, wear slippers around the house, and only use a fan on my feet in the evening before bed. I still had flares, but the pain was much more tolerable. However, the treatments themselves were extremely painful, and I had to stop after about six weeks.
During much of this time, I have been housebound and unable to walk due to my TTS. There was a period of nearly two years when I recovered enough to walk a little bit and leave the house occasionally. Then I had a relapse and am back to being unable to walk again. EM and TTS have both caused me to become very isolated. I am fortunate to have a wonderful husband and son who take good care of me. I have struggled with depression throughout my illness but am finally learning to manage it by finding some new hobbies and focusing on the things I can still do that bring me joy.
Stephen Hawking: “However bad life may seem, there is always something you can do and succeed at. Where there’s life, there’s hope.”

Patricia Michaux
I hope I can help others by sharing my story. I have had EM in my feet for ten years, when I walk after about 1 km (approximately 2/3 of a mile). My husband and I recently stayed in Lisbon, Portugal. To see more of the city, we walked a lot and my feet really suffered. When I returned to Paris, I went back to the doctor who diagnosed my illness earlier.
He performed a Doppler test and the result was that the Doppler remained silent when on my feet. When he put it on my hands, it made a normal buzzing sound. It looked as if there was no blood circulation in my feet and that they were dead.
He prescribed a daily dose of Tildiem (dilitiazem*) 60 mg, saying it could take a few months to work. After three weeks, I noticed a real improvement. I can walk for a long time without pain. I also noticed that my feet, which had become increasingly rigid, began to be more flexible and my ankles less painful during rotation. I’ve been taking this for over two months and now walk as much as I want. Tildiem has changed my life.
